Podcast: Play in new window | Download
 Sleep is extremely important for the whole body. The brain is no exception. When we are recovering from PTSD we need are brains firing on all cylinders.
Sleep is extremely important for the whole body. The brain is no exception. When we are recovering from PTSD we need are brains firing on all cylinders.
PTSD introduces some difficult barriers to sound sleep. Hyper-vigilance and nightmares are two obstacles that those with PTSD face.
However, a good night’s rest starts with the same foundation for both those with PTSD and the rest of the population. Once the foundation is in place we are better equipped to deal with specific difficulties.
The foundation
Several sleep improvements list exist. I link to a few of them below. Here are the 10 things I have found helpful.
1. Get plenty of light.
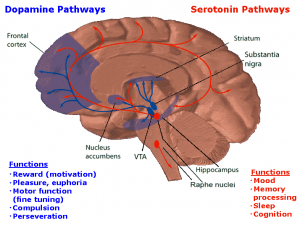
What? I thought dark was necessary for sleep? Well, it is. However, getting plenty of intense light in the morning can help set of up for sleep at night. Daylight intensity triggers our brain to produce serotonin—an important brain chemical, especially during the day, for emotions, thinking and energy. It is made by the same gland in the brain that produced melatonin—an important brain chemical for nighttime for rest that is produced in the dark.
2. Get plenty of physical activity.
Yes, that beloved topic…exercise! Exercise is excellent for reducing stress and balancing out brain chemicals. It is usually best to do it early in the day or at least 4 hours before bed. Your body needs time to cool down and recover.
3. Make sure it is dark.
Just as we need light during the day to help our brains fully function. We need dark to help the properly function while we sleep (see above).
Experiment with getting rid of as much light as possible. Sometimes window blinds are not enough. Curtains over windows (or experiment with putting up a thick blanket.) Clock radios, cell phones, cordless phones, chargers, and other electronics can also be a source of light that might affect our brain activity.
The experts also say the light from TV or computer screens can interfere with melatonin production.
4. Limit or Eliminate Caffeine
It is a stimulant. People often report that it does not affect their sleep. It may not may or may not affect your ability to fall asleep. But it does affect your ability to get the proper rest your brain needs.
At the very least limit your caffeine intake to 1 or 2 servings a day. Stop caffeinated beverages around 2 pm (about 8 hours before bed).
5. Eliminate Nicotine
It is a stimulant.
6. Limit Alcohol
Alcohol is a depressant and it can help someone fall asleep. However, it interferes the deep, restful and restorative stages 3 and 4 of the sleep cycle. In other word, you may fall asleep more quickly but you will not rest as soundly.
7. Watch what and when you eat.
A big meal may make you sleepy but it won’t typically give you a good night’s rest. Digesting a heavy or spicy meal has been shown to interfere with a good night sleep. Try eating a litter earlier in the evening. Consider making dinner a smaller meal. Reserve lunch for the spicy or heavy foods.
8. Limit your activity in bed.
Reserve this space for sleep and sex. From stress to mental stimulation, E-mail, work, electronics each can disrupt our rest.
These last two may be particularly helpful for those with PTSD.
9. Meditation and deep breathing
Practice these techniques during the day. If necessary apply them as you are trying to get your mind in a restful state around bed time. Once learned, these can also be useful with we become overstimulated—loud noise, dream, etc.
10. Medication for nightmare reduction instead of a direct sleep aid.
If nightmares are a problem talk with your healthcare provider. For a long time I use a medication called Prazosin. It is an older blood pressure medication. My provider told me that it was about 80% effective in a double blind study at reducing or eliminating nightmares in PTSD patients.
It was affective for me as well. But be careful. It can seriously lower your blood pressure—especially as your body adjust to the increasing dose. So take care when you rise at night, especially to use the bathroom.
It worked for me. While I was taking Prazosin I hardly had a nightmare.
So why did I stop? I experienced one of the rarer side effect, nocturnal enuresis…aka nighttime urinary incontinence or bed-wetting.
Yet I am glad I took it for a while. It helped me get better sleep. The better sleep helped me better deal with the underlying problems. From time to time I still have PTSD related nightmares, but they are getting less intense and lest frequent.
Question: What has helped you get a healthy, restful and restorative night sleep?
Some Sleep Resources
- UCLA Health: Sleeping Well to Live Well
- Psychology Today: New Details on Caffeine’s Sleep-Disrupting Effects
- WSU: Does Drinking Alcohol Affect Sleep?
- WebMD: Prazosin for PTSD